Facts & Stats
Learn more about osteoporosis and related fractures
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue which can lead to increased risk of fracture.
Known as the “silent thief”, bone deterioration can occur over a number of years without any symptoms. Unfortunately, by the time affected bones break or fracture, the disease is already fairly advanced and less treatable.
The most common fractures associated with osteoporosis are in the hip, spine, wrist, and shoulder.
Today, no single cause for osteoporosis has been identified.
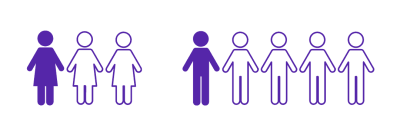
At least 1 IN 3 WOMEN and 1 IN 5 MEN will suffer from an osteoporotic fracture during their lifetime
OVER 80% OF ALL FRACTURES in people 50+ are caused by osteoporosis
Bone health is important at every age but especially during childhood and adolescence when bones are still growing. As most people reach their maximum bone size and strength (known as peak bone mass) by age 30, bone-healthy behaviours are important from an early age in order to optimize bone health and reduce the risk of developing osteoporosis later in life.
Women and men alike BEGIN TO LOSE BONE IN THEIR MID-30S
22% OF WOMEN and 33% OF MEN who suffer a hip fracture will die within one year
ONE IN THREE HIP FRACTURE PATIENTS will re-fracture within one year
Women and men alike BEGIN TO LOSE BONE IN THEIR MID-30S
22% OF WOMEN and 33% OF MEN who suffer a hip fracture will die within one year
ONE IN THREE HIP FRACTURE PATIENTS will re-fracture within one year
Learn more
- Osteoporosis is a condition that causes bones to become thin and porous, decreasing bone strength and leading to increased risk of breaking a bone.
- No single cause for osteoporosis has been identified.
- Osteoporosis can strike at any age.
- Osteoporosis affects both men and women.
- Osteoporosis is often called the ‘silent thief’ because bone loss occurs without symptoms unless one has fractured.
- At least 1 in 3 women and 1 in 5 men will suffer from an osteoporotic fracture during their lifetime.
- Bone health is important at every age but especially during childhood and adolescence when bones are still growing. As most people reach their maximum bone size and strength (known as peak bone mass) by age 30, bone-healthy behaviours are important from an early age in order to optimize bone health and reduce the risk of developing osteoporosis later in life. *
- Reduce the risk of bone loss by following a healthy lifestyle with balanced nutrition, ideally starting from childhood.
- Over 2.3 million Canadians are living with osteoporosis.
- Over 80% of all fractures in people 50+ are caused by osteoporosis.
- 1 in 3 hip fracture patients will re-fracture within one year.
- Women and men alike begin to lose bone in their mid-30s.
- 22% of women and 33% of men who suffer a hip fracture will die within one year. *
- The most common sites of osteoporotic fracture are the wrist, spine, shoulder and hip.
- Fractures from osteoporosis are more common than heart attack, stroke and breast cancer combined.
- The overall annual cost to the healthcare system is estimated at over $4.6 billion due to improved data capture of the multiple encounters and services that accompany a fracture: emergency room, admissions to acute and step-down non-acute institutions, rehabilitation, home-assisted or long-term residency support. *
- Osteoporosis causes 70-90% of 30,000 hip fractures annually.
- The average cost to the healthcare system in the first year following a hip fracture is $63,649. For hip fracture patients who cannot be discharged back home and who require admission to a long-term care facility, the average cost to the healthcare system in the first year following that broken hip is $125,085. *
- Osteoporotic hip fractures consume more hospital bed days than stroke, diabetes, or heart attack.
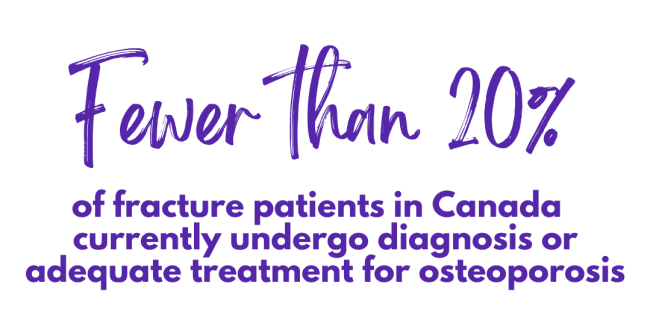
- Fewer than 20% of fracture patients in Canada currently undergo diagnosis or adequate treatment for osteoporosis.
- 80% of patients with a history of fractures are not given osteoporosis therapies. Hundreds of thousands of Canadians needlessly fracture each year because their osteoporosis goes undiagnosed and untreated.
- After sustaining a common osteoporotic fracture, less than 10% of Canadians aged 40+ had their BMD measured.
- A study recently reported that only 44% of people discharged from hospital for a hip fracture return home; of the rest, 10% go to another hospital, 27% go to rehabilitation care, and 17% go to long-term care facilities.
- 14% of persons with a wrist fracture suffered a repeat fracture within 3 years.
- Over 1 in 2 hip fracture patients will suffer another fracture within 5 years.
- As women approach menopause, they lose bone at a greater rate, from 2-3 per cent per year.
- The risk of suffering a second spine fracture within the first 12 months following an initial vertebral fracture is 20%
- About 80% of those living with diagnosed osteoporosis are women.
- In 2016–2017, there were 150 hip fractures per 100,000 Canadians aged 40+.
- Women were 2x more likely to fracture their hip compared to men.
- Men being 1.3x more likely to die from any cause following a hip fracture.
- Osteoporosis can result in disfigurement, lowered self-esteem, reduction or loss of mobility, and decreased independence.
- Risk factors include older age, sex, vertebral compression fracture, fragility fracture after age 40, either parent has had a hip fracture, >3 months use of glucocorticoid drugs, medical conditions that inhibit absorption of nutrients and other medical conditions or medications that contribute to bone loss.
- Loss of 2cm (3/4″) as measured by one’s healthcare provider or 6cm (2 1/2″) overall from when one was younger may be an indicator of spinal fracture.
The Osteoporosis Care Gap
- After sustaining a common osteoporotic fracture, less than 20% of Canadians aged 65+ were prescribed a treatment for osteoporosis.
- After sustaining a common osteoporotic fracture men are less likely to receive any intervention.
- BONE ATTACK <25% that had a hip fracture received medication to prevent a future fracture VS HEART ATTACK 80% received medication to prevent a future heart attack
- Given the success Fracture Liaison Service (FLS) is having in preventing secondary fractures and the resulting cost-saving benefits – increasing accessibility to FLS across the country will help to close the existing osteoporosis care gap. *
* Access the 2022 Osteoporosis Facts and Stats document including appendix here.
Osteoporosis Canada has been working closely with the Public Health Agency of Canada (PHAC) over the past few years assisting in the collection of data in Canada’s Canadian Chronic Disease Surveillance System (CCDSS).