Healthy Bones and Healthy Swallowing: Nutritional Strategies for Dysphagia

Healthy Bones and Healthy Swallowing: Nutritional Strategies for Dysphagia
What is dysphagia?
People living with dysphagia have difficulties with swallowing, which may impact their nutrition, hydration and ability to take certain medications.
Although we may take our ability to swallow for granted, it is a complicated and well-coordinated process involving many different body parts.
| Interesting tidbit: Swallowing requires the concerted actions of many pairs of muscles and cranial nerves (nerves in the skull). Under normal circumstances we swallow about 500 to 2000 times daily (food, liquid and saliva). |
When we eat, swallowing starts in the mouth, where food is chewed, and then moistened and softened with the addition of saliva. Subsequently, food and/or liquids are moved to the back of the mouth towards the throat, and into the esophagus (food pipe). They are then pushed down the esophagus, in a well-coordinated manner, into the stomach. At the same time, our body prevents food from going to the wrong places: coming out our nose, going down our airway, or moving in the wrong direction (back up from the stomach).
Diseases affecting the brain, nerves and muscles may impair the action or control of the swallowing process, causing food and/or liquids to get “stuck” or “misdirected” anywhere along the process, anywhere from the mouth to the esophagus.
Blockages, such as due to cancer, or narrowing of the esophagus, may also cause dysphagia, as the flow of food/liquids is restricted.
Your health care provider will review your medical history and the history of your symptoms, and perform a focused physical examination to help find the cause of your dysphagia. You may be referred to a speech-language pathologist, who is a clinical expert in the diagnosis and treatment of dysphagia. You may need a swallowing assessment, which is sometimes done with the help of x-rays and instruments to look at the structures involved.
- Instrumental swallowing tests include those that involve x-rays, such as modified barium swallows / videofluoroscopic swallowing studies, or those that involve the use of an endoscope with a light and camera, such as flexible endoscopic evaluation of swallowing.
- Each test has different strengths and weaknesses, and one or both may need to be used in different circumstances.
- These tests can observe what happens when you swallow food and drinks, and how certain maneuvers affect your anatomy and physiology.
- Results of these exams provide your speech-language pathologist a basis on which to recommend swallowing treatment and rehabilitation.
Living with dysphagia
There are many strategies to ensure adequate nutrition and hydration despite swallowing difficulties. Some of these include: strengthening muscles used for chewing and swallowing, ensuring proper positioning during eating, employing strategies to help facilitate swallowing and airway protection, and modifying diet textures to help optimize the safety and efficiency of swallowing.
Not all those living with dysphagia need diet alterations. For those who may benefit from diet alterations, many types of textures may be recommended, ranging from thin and thickened drinks, to foods that are pureed, minced and moist, soft and bite-sized, or regular texture. The choice of food texture for a person needs to be individualized, after careful assessments by a speech-language pathologist and/or a dietitian. Ideally, an alteration in diet consistency, particularly a change in liquid consistency, should be informed by a swallowing study. Long-term use of altered diets in the absence of appropriate follow-up can lead to malnutrition, dehydration, and loss of quality of life.
What are the nutritional needs for good bone health?
For postmenopausal women and men over 50 years old, Osteoporosis Canada recommends following Health Canada’s recommendation regarding adequate nutritional intake for good bone health.
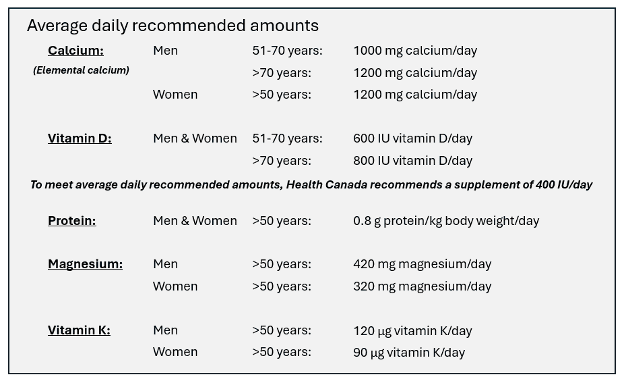
Adapted from Table 2, Appendix 1, Osteoporosis Canada 2023 Guideline
Source: Health Canada
- https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/dietary-reference-intakes/tables/reference-values-elements.html
- https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/dietary-reference-intakes/tables/reference-values-vitamins.html
- https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/dietary-reference-intakes/tables/reference-values-macronutrients.html
To determine the quantity of each nutrient in one serving of food or beverage, please consult with Osteoporosis Canada’s Nutrient Calculator.
For example:
| Calcium | Vitamin D | Protein | Magnesium | Vitamin K | |
| Milk, skim (1 cup) | 316 mg | 2.6 μg = 104 IU | 9.0 g | 28 mg | 0 μg |
| Soy beverage, fortified (1 cup) | 319 mg | 0.80 μg = 32 IU | 4.2 g | 31 mg | 0 μg |
| Egg, large (1) | 24 mg | 0.81 μg = 32.4 IU | 6.3 g | 5 mg | 0.12 μg |
| Yogurt beverage, with vitamin D added (200 mL) | 168 mg | 1.28 μg = 51.2 IU | 5.26 g | 17 mg | 0 μg |
| Banana, medium (1) | 6 mg | 0 IU | 1.0 g | 32 mg | 32 μg |
People living with dysphagia may benefit from food and beverages of different textures, to improve swallowing efficiency, safety, or both. However, nutrient-rich ingredients do not need to be compromised with these modified diets!
Below are some suggestions of dietary calcium, vitamin D, protein, magnesium and vitamin K, as per different liquid and food textures. Be aware that eating foods that are not recommended on one’s “dysphagia diet” may increase the risk of swallowing problems and aspiration. Please consult with a speech-language pathologist and a dietitian to determine which liquid/food textures and food items may be most appropriate.
Food textures and drink thickness are described using standard terminology from the International Dysphagia Diet Standardisation Initiative (IDDSI). This consists of a scale of 8 levels, ranging from level 0 (thin fluids), to level 7 (regular, easy to chew foods). Foods and drinks are stratified by characteristics like particle size, moisture, stickiness, and softness.
Description of different textures of drinks and foods:
| Thin fluids (IDDSI 0) | Flows like water Fast flow Can drink through any type of cup or straw as appropriate for age and skills |
| Slightly thick fluids (IDDSI 1) | Thicker than water Requires a little more effort to drink than thin liquids Flows through a straw or syringe |
| Mildly thick fluids (IDDSI 2) | Flows off a spoon Sippable, pours quickly from a spoon, but slower than thin drinks Mild effort is required to drink this thickness through standard bore straw (standard bore straw = 5.3 mm diameter) |
| Moderately thick fluids or liquidised foods (IDDSI 3) | Can be drunk from a cup Moderate effort is required to suck through a standard bore or wide bore straw (wide bore straw = 6.9 mm) Cannot be piped, layered or molded on a plate because it will not retain its shape Cannot be eaten with a fork because it drips slowly in dollops through the prongs Can be eaten with a spoon No oral processing or chewing required – can be swallowed directly Smooth texture with no ‘bits’ (lumps, fibers, bits of shell or skin, husk, particles of gristle or bone) |
| Extremely thick fluids or pureed foods (IDDSI 4) | Usually eaten with a spoon (a fork is possible) Cannot be drunk from a cup because it does not flow easily Cannot be sucked through a straw Does not require chewing Can be piped, layered or molded because it retains its shape, but should not require chewing if presented in this form Shows some very slow movement under gravity but cannot be poured Falls off spoon in a single spoonful when tilted and continues to hold shape on a plate No lumps Not sticky Liquid must not separate from solid |
| Minced & moist foods (IDDSI 5) | Can be eaten with a fork or spoon Could be eaten with chopsticks in some cases, if the individual has very good hand control Can be scooped and shaped (e.g. into a ball shape) on a plate Soft and moist with no separate thin liquid Small lumps visible within the food (equal to or less than 4mm width and no longer than 15mm in length) Lumps are easy to squash with tongue82 |
| Soft & bite-sized foods (IDDSI 6) | Can be eaten with a fork, spoon or chopsticks Can be mashed/broken down with pressure from fork, spoon or chopsticks A knife is not required to cut this food, but may be used to help load a fork or spoon Soft, tender and moist throughout but with no separate thin liquid Chewing is required before swallowing ‘‘Bite-sized’ pieces as appropriate for size and oral processing skills (no longer than 15 mm) |
| Regular, easy to chew foods (IDDSI 7) | Normal, everyday foods of soft/tender textures that are developmentally and age appropriate Any method may be used to eat these foods Sample size is not restricted at Level 7, therefore, foods may be of a range of sizes Does not include: hard, tough, chewy, fibrous, stringy, crunchy, or crumbly bits, pips, seeds, fibrous parts of fruit, husks or bones May include ‘dual consistency’ or ‘mixed consistency’ foods and liquids if also safe for Level 0, and at clinician discretion. If unsafe for Level 0 Thin, liquid portion can be thickened to clinician’s recommended thickness level |
Dietary sources of calcium, vitamin D, protein, magnesium and vitamin K, as per different textures.
| Calcium | Vitamin D | Protein | Magnesium | Vitamin K | |
| Thin fluids (IDDSI 0) | Milk, fortified orange juice (with no pulp), fortified soy/almond/rice beverages | Milk, fortified orange juice (with no pulp), fortified soy/almond/rice beverages | Milk, soy beverages | Milk, soy beverages, orange juice, watermelon juice | Carrot juice, pomegranate juice, cherry juice |
| Slightly thick fluids (IDDSI 1) | Nutritional supplement, fortified orange juice (with no pulp), milk, fortified soy/almond/rice beverages | Fortified orange juice (with no pulp), milk, fortified soy/almond/rice beverages | Meal replacement beverages, milk, soy beverages | Milk, soy beverages | Fortified meal replacement beverages |
| Mildly thick fluids (IDDSI 2) | Full fat milk | Full fat milk | Full fat milk | Full fat milk | |
| Note: Some smoothies, milkshakes, and yogurt drinks may be mildly thick and can be enjoyed without adding thickener. Most liquids will need a thickener added, however. | |||||
| Moderately thick fluids or liquidised foods (IDDSI 3) | Smooth yogurt | Smooth yogurt, egg custard | Smooth yogurt, egg custard | Smooth yogurt | |
| Note: Thin fluids (IDDSI 0) can be thickened with thickening powders or gels. Using different amounts of thickening agents may result in fluids of different textures (IDDSI 1 to 4) Also, thickened fluids should remain thick at room temperature. Some ice cream, sherbet, Jello and popsicles melt at room temperature, and may not be safe to consume for those restricted to thickened fluids. If in doubt, the item should be tested at room temperature. | |||||
| Extremely thick fluids or pureed foods (IDDSI 4) | Yogurt, kefir, cream soups, pudding | Yogurt, cream soups | Yogurt, kefir, pureed green peas, pureed meat/fish | Pureed bananas, pureed baked beans, pureed spinach, pureed avocado, soft silken tofu | Pureed leafy green vegetables (spinach kale, collard greens), pureed carrots, pureed kiwi, pureed pumpkin, pureed broccoli |
| Note: Most foods can be pureed and made into the right consistency by adding fluid (water, broth, milk, etc.). Meats that are to be pureed should be cooked with moisture (boiled, poached, steamed or braised). | |||||
| Minced & moist foods (IDDSI 5) | Cottage cheese, custard | Boiled/poached fatty fish, egg salad | Mashed green peas, mashed beans and legumes, hummus, finely ground meats served with sauce to further moisten and soften food, egg salad, mashed fish | Mashed bananas, hummus | Mashed blueberries, mashed bananas |
| Soft & bite-sized foods (IDDSI 6) | Soft cheeses | Scrambled eggs, poached eggs, egg salad | Scrambled eggs, poached eggs, egg salad, tender meats, soft fish | Ripe bananas, soft tofu | Blueberries, ripe bananas |
| Regular, easy to chew foods (IDDSI 7) | Fortified tofu | Eggs, soft fatty fish, fortified tofu | Soft meats or fish, tofu, eggs | Tofu, bananas | Vegetables (spinach, kale, collard greens, carrots, broccoli, iceberg lettuce), fruits (bananas, blueberries, kiwi, pumpkin) |
| Note: Although there are no restrictions on the size of food particles for IDDSI 7, certain types of textures should be avoided. These include foods that are hard, tough, chewy, sticky, fibrous, stringy, or foods that may contain crunchy or crumbly bits, pips or seeds, fibrous parts of fruit, husks or bones. | |||||
Note: Certain foods can fall into different IDDSI categories depending on their consistency/texture. These may differ by brand for store-bought items. Cooking methods (amount of moisture added, amount of time cooked, cooking style) may also affect the IDDSI level of foods.
Supplements
Ideally, calcium, protein, magnesium and vitamin K requirements can be achieved through diet alone. Consult with Osteoporosis Canada’s Nutrient Calculator to gauge the nutrient content in various foods.
However, when the recommended targets cannot be met from diet alone, supplementation may be helpful.
Calcium and Magnesium:
Although calcium or magnesium supplements are mostly in pill form, liquid versions of these supplements are also available. For those who cannot swallow thin liquids, thickening agents can be added to create the desired texture.
Vitamin D:
A supplement of vitamin D is likely required, as natural and dietary sources will be inadequate. In fact, Health Canada recommends that all adults over age 50 take a daily vitamin D supplement of 400 international units (IU) per day to help meet our vitamin D needs.
For those who are unable to swallow vitamin D pills, liquid vitamin D, or dissolvable vitamin D tablets may be options. Given the concentration of liquid vitamin D, only a few drops would be needed. These can be dropped directly into the mouth, or mixed with a spoonful of texture appropriate liquid or food.
Protein:
There are a variety of protein supplements, from protein shakes to protein powders. The thickness of these products differs by brand, and by the amount of liquid added to them. Given the great variation in these classes of products, the appropriate choice of supplement should be reviewed with a speech language pathologist or a dietitian.
Vitamin K:
Similar to vitamin D, supplements of vitamin K are available as pills or capsules, but also as drops or dissolvable tablets.
Which osteoporosis medications are safe for those living with dysphagia?
For those who, after careful consideration and discussion with their health care provider, need medication to help treat their osteoporosis, a medication family known as oral bisphosphonates is usually the first prescription medication treatment. This involves a pill, usually taken once weekly. However, this pill cannot be crushed and mixed with foods, as the pill has a special coating to optimize its absorption.
For those living with dysphagia, there is a chance that this pill may get stuck anywhere in between the mouth and the esophagus. If this pill gets stuck in the esophagus, serious complications may occur, such as inflammation, irritation, or damage to the esophagus. The pill may also be aspirated (get into the lungs), which may result in pulmonary complications.
For those living with dysphagia who require medication to optimize their bone health, a non-pill option would be ideal. There are several options including injection and infusion (intravenous or IV) medications. Speak with your health care provider to determine which option may be best for you.
Although there may be many challenges and adaptations to daily routines, health does not need to be compromised for those living with dysphagia. A balanced diet prepared appropriately can provide the adequate nutrients needed for bone health and overall wellness. Contact speech-language pathologists and dietitians, or visit their websites, to learn more about dysphagia and treatment plans.
How can I access a Speech-Language Pathologist or a Dietitian?
- For some individuals, your first encounter with a speech-language pathologist or a dietitian may be in the hospital, when dysphagia is first diagnosed.
- More commonly, dysphagia is diagnosed in an outpatient office or clinic. Your primary care provider can refer you to an outpatient speech-language pathologist or dietitian, but referrals are usually not necessary. However, if you have a private health insurance plan, the insurance company may require a referral from your primary care provider, before reimbursements are provided.
- You can find a speech-language pathologist through Speech-Language & Audiology Canada’s website: https://member-membre.sac-oac.ca/search/custom.asp?id=7109
- You can find dietitians in private practice through Dietitians of Canada’s website: https://members.dietitians.ca/Web/Web/Membership/Directory/Find_a_Dietitian_Directory.aspx
Resources:
- Learn more about dysphagia:
- Dysphagia: https://www.sac-oac.ca/wp-content/uploads/2024/06/Info-Sheet-Dysphagia-EN-Digital.pdf
- The Role of Speech-Language Pathologists in Dysphagia: https://www.sac-oac.ca/wp-content/uploads/2023/02/dysphagia_position_statement_en.pdf
- Swallowing problems (Dysphagia): https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Pages/brochure.aspx?itemid=564
- Learn more about different dysphagia diets:
- Pureed Foods and Thickened Liquids: https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Pages/brochure.aspx?itemid=1454
- Minced and Moist Foods: https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Pages/brochure.aspx?itemid=1488
- Soft and Bite-Sized Foods: https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Pages/brochure.aspx?itemid=14
- Easy to Chew Foods: https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Pages/brochure.aspx?itemid=15
- Complete International Dysphagia Diet Standardisation Initiative (IDDSI) Framework: https://cms.iddsi.org/media/publications-iddsi/detaileddesriptions/english/V2DetailedDefnEnglish31july2019.pdf
- Speech-Language & Audiology Canada: https://www.sac-oac.ca/
- Dietitians of Canada: https://www.dietitians.ca/
- Osteoporosis Canada’s Nutrient Calculator: https://osteoporosis.ca/nutrient-calculator/
Credit:
Adrienne Mak, Honours Bachelor of Arts (prospective Speech-Language Pathology student)
Kerry Grady, Senior Manager, Clinical & Education Programs, Osteoporosis Canada
Adrian Lau, Endocrinologist, Women’s College Hospital; Vice Chair, Scientific Advisory Council, Osteoporosis Canada
Reviewed by:
Jennifer Cameron-Turley, Interim Director of Speech-Language Pathology and Communication Health Assistants, Speech-Language & Audiology Canada
Deidre Burns, Clinical Dietitian in Inpatient Care & Dysphagia Management, Nova Scotia Health Authority
Wendy Ward, Chair, Nutrition Working Group, 2023 Osteoporosis Clinical Practice Guideline
COPN Review Committee (Joanna Sale, Laura Rothman, Teri Charrois, Zahra Bardai)
COPN Executive Committee (Jackie Herman, Tammy Clark)
(COPN, the Canadian Osteoporosis Patient Network is the patient arm of Osteoporosis Canada, a national network of people living with osteoporosis.)