
Discontinuation of Denosumab FAQ

Discontinuation of Denosumab FAQ
Authors: Dr. Adrian Lau, Dr. Laura Rothman, Dr. Joanna Sale, Dr. Jenny Thain, Dr. Teri Charrois
Recommendations from Osteoporosis Canada Rapid Response Team.
Many Canadians are taking denosumab injections for their bone health. However, there are some uncertainties about the use of this injectable osteoporosis medication.
How often do I need denosumab?
- Denosumab can be very effective in reducing fracture risk, and maintaining bone mineral density. However, in order to maintain these benefits, denosumab has to be administered without any interruptions.
- Denosumab should be given once every 6 months. It is safe if the dose is slightly delayed, but not more than 7 months after the previous dose.
- If a dose is delayed beyond 7 months after the previous dose, there is an increased risk of rapid bone loss and multiple vertebral fractures.
- Remember to plan your doses ahead of time, with your pharmacy, and healthcare professional who is administering your dose. You may also need to plan your doses around the time you may be out of town.
How long can I be on denosumab therapy?
- Once you have started on denosumab therapy, it is recommended that you continue the therapy for the “long-term”.
- The optimal duration of denosumab therapy is debatable. Research studies have shown denosumab therapy to be effective for up to 10 years. However, beyond 10 years, there is less data available. Talk with your physician about the optimal duration of therapy for you, as this may depend on factors specific to you.
Can I take denosumab indefinitely (forever)?
- We do not know the answer to this. There is little data about treatment with denosumab beyond 10 years.
- From current data, there appears to be an increased risk of rare side effects with prolonged, uninterrupted use of denosumab. These risks may increase with longer duration of use of denosumab.
- These rare side effects include atypical femur fractures (AFFs) and osteonecrosis of the jaw (ONJ).
- Hence, the decision about the duration of your therapy is a balance between the benefits (reduced fracture risk, maintained bone density), and potential harms (rare side effects) of ongoing therapy.
- Since the optimal duration of therapy is unknown, it is best to consult with your health care professional to determine what is best for your circumstances.
If I need to stop denosumab therapy, how can I do it safely? I was told that stopping denosumab therapy may result in significant bone loss and increased risk of spine fractures.
- Some people may choose to stop denosumab therapy because they are experiencing side effects, or if they would like to reduce their risk of AFFs or ONJ with ongoing therapy.
- There is evidence that suddenly stopping denosumab therapy can result in rapid decline in bone density and the development of new spine fractures.
- There are strategies that may help decrease the risk of these adverse outcomes. The optimal strategy for this is still unknown and is an ongoing area of research.
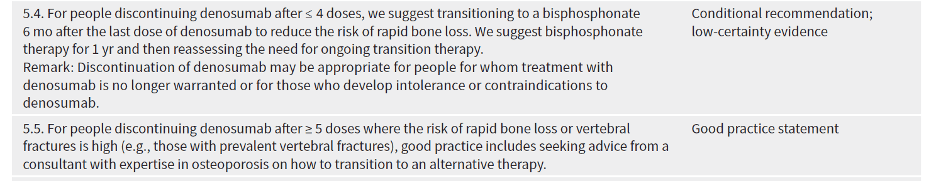
- In the 2023 Osteoporosis Canada Guideline, two recommendations are made, depending on how long you have been on denosumab for:
When I stop denosumab, do I need oral or intravenous (IV) bisphosphonate?
- The decision to use an oral or IV bisphosphonate may depend on many factors, including personal preference, the duration of your denosumab therapy, and your previous tolerance to bisphosphonate therapy.
- This decision should be made between you and your physician, based on your preference and considering the factors stated above.
Do I need more frequent bone mineral density testing or special blood tests (such as bone turnover markers) when I transition off denosumab therapy?
Your physician will help you with the transition off denosumab, including any investigations that are necessary. In some situations, your physician may refer you to a specialist with expertise in osteoporosis for a second opinion.
A repeat bone mineral density test (DXA scan) is necessary after stopping denosumab. However, the ideal timing for this test may differ for different people, and this decision should be discussed with your physician.
There is debate about whether checking bone turnover markers is helpful. This is a blood test that may not be readily available to all individuals, and its cost may or may not be covered by provincial/territorial health plans.
Scientific Advisory Council
Osteoporosis Canada’s rapid response team, made up of members of the Scientific Advisory Council, creates position statements as news breaks regarding osteoporosis. The position statements are used to inform both the healthcare professional and the patient. The Scientific Advisory Council (SAC) is made up of experts in Osteoporosis and bone metabolism and is a volunteer membership.


