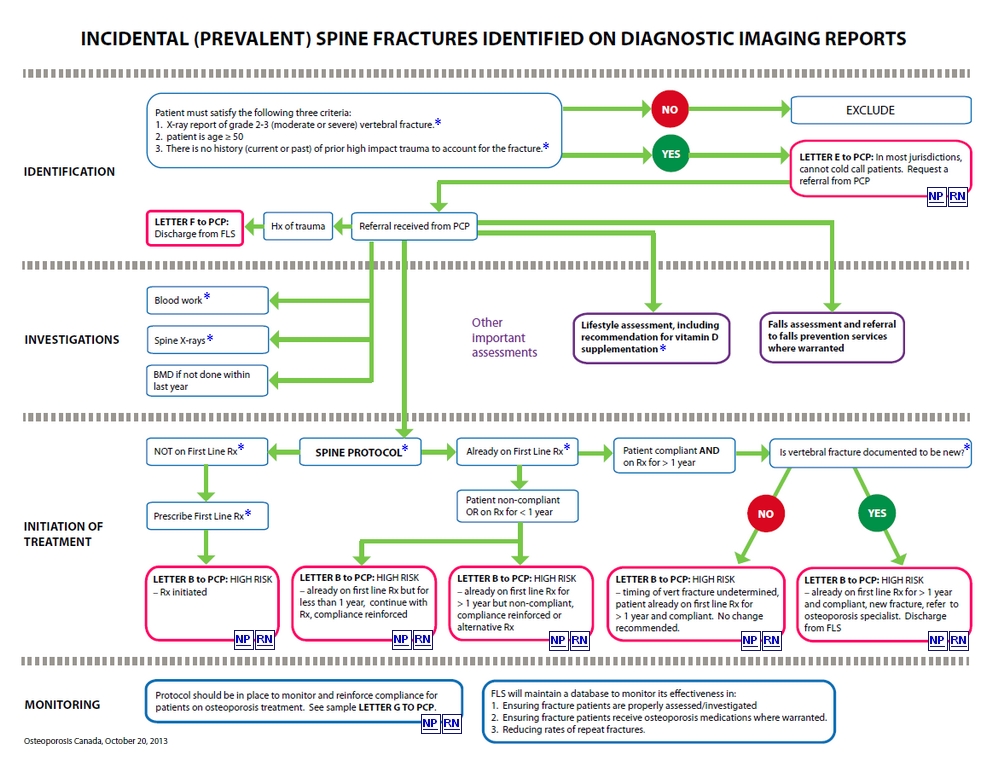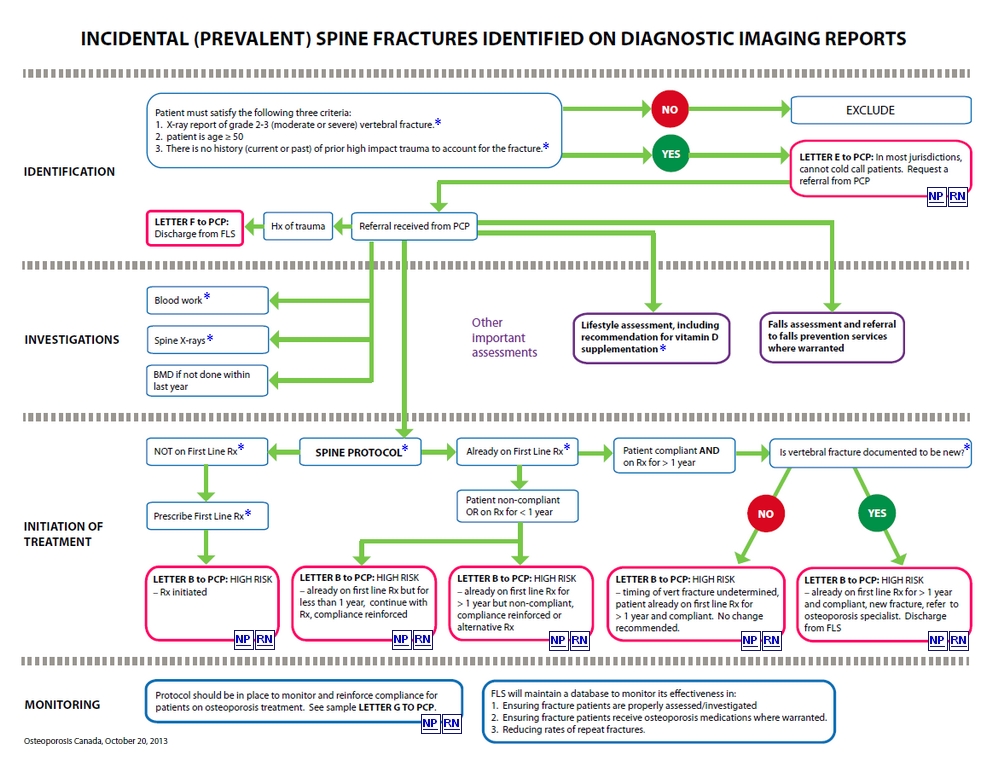
Spine
fractures are often discovered incidentally on diagnostic imaging
studies that were done for other medical reasons (e.g. chest x-rays,
lumbar spine x-rays, CT of chest or abdomen, MRI of chest or abdomen
etc.). Provided radiologists can agree in advance to consistent
definitions and terminology, spine fractures that are indicative of
underlying osteoporosis can become readily identified by an FLS through
scanning of diagnostic imaging reports. As per Osteoporosis
Canada’s Guidelines , Grade II (26-40%) and Grade III
(> 40%) spine fractures according to Genant’s
semi-quantitative classification should receive the greatest attention.
OC and the Canadian Association of Radiologists are currently
developing consistent terminology for spine fractures. Once this
becomes published, the FLS working group will update these
recommendations.
When
a vertebral fracture is incidentally identified on x-ray, it is
important to distinguish if it was due to fragility or other causes
(such as trauma, metastatic disease etc.). If the vertebral fracture
was due to fragility, then the individual is deemed to suffer from
osteoporosis; if it was due to other causes, then osteoporosis
treatment may not be warranted. For this reason, one must elicit any
prior history of major trauma that could explain the origin of the
fracture. Some patients may already be aware that they have a vertebral
fracture because of previous high impact trauma or they may be able to
provide information of severe high impact trauma in the past which may
have caused a vertebral fracture that was not identified at the time
(e.g. major motor vehicle accident causing back pain and patient was
bedridden for two weeks but no x-rays were done or available from that
incident). If, however, the historical details are ambiguous, referral
to an osteoporosis specialist may then be warranted.
Recommended
biochemical tests for patients being assessed for osteoporosis as per
the 2010 OC Guidelines: serum calcium corrected for albumin or ionized
calcium, complete blood count (CBC), creatinine or eGFR, alkaline
phosphatase, thyroid stimulating hormone (TSH). For patients with
vertebral fractures, a serum protein electrophoresis is also
recommended. Vitamin D (25-hydroxy vitamin D) should be measured after
3-4 months of adequate supplementation and should not be repeated if
optimal level ≥ 75 nmol/L is achieved.
The
IOF Best Practice Framework indicates that patients with any fragility
fracture should be assessed for the presence of spine fractures. This
requires a lateral view of the thoracic and lumbar spine, typically by
conventional x-rays or, where available, by Vertebral Fracture
Assessment (VFA) by DXA. If the initial presenting fracture is a
vertebral fracture, it is important to ensure that the entire spine is
imaged (e.g. if a T10 fracture is identified on a lateral chest x-ray,
then a lateral view of the lumbar spine is also indicated).
When
a vertebral fracture is incidentally identified on x-ray, it is
important to distinguish if it was due to fragility or other causes
(such as trauma, metastatic disease etc.). If the vertebral fracture
was due to fragility, then the individual is deemed to suffer from
osteoporosis; if it was due to other causes, then osteoporosis
treatment may not be warranted. For this reason, one must elicit any
prior history of major trauma that could explain the origin of the
fracture. Some patients may already be aware that they have a vertebral
fracture because of previous high impact trauma or they may be able to
provide information of severe high impact trauma in the past which may
have caused a vertebral fracture that was not identified at the time
(e.g. major motor vehicle accident causing back pain and patient was
bedridden for two weeks but no x-rays were done or available from that
incident). If, however, the historical details are ambiguous, referral
to an osteoporosis specialist may then be warranted.
Recommended
biochemical tests for patients being assessed for osteoporosis as per
the 2010 OC Guidelines: serum calcium corrected for albumin or ionized
calcium, complete blood count (CBC), creatinine or eGFR, alkaline
phosphatase, thyroid stimulating hormone (TSH). For patients with
vertebral fractures, a serum protein electrophoresis is also
recommended. Vitamin D (25-hydroxy vitamin D) should be measured after
3-4 months of adequate supplementation and should not be repeated if
optimal level ≥ 75 nmol/L is achieved.
The
IOF Best Practice Framework indicates that patients with any fragility
fracture should be assessed for the presence of spine fractures. This
requires a lateral view of the thoracic and lumbar spine, typically by
conventional x-rays or, where available, by Vertebral Fracture
Assessment (VFA) by DXA. If the initial presenting fracture is a
vertebral fracture, it is important to ensure that the entire spine is
imaged (e.g. if a T10 fracture is identified on a lateral chest x-ray,
then a lateral view of the lumbar spine is also indicated).
When
a vertebral fracture is incidentally identified on x-ray, it is
important to distinguish if it was due to fragility or other causes
(such as trauma, metastatic disease etc.). If the vertebral fracture
was due to fragility, then the individual is deemed to suffer from
osteoporosis; if it was due to other causes, then osteoporosis
treatment may not be warranted. For this reason, one must elicit any
prior history of major trauma that could explain the origin of the
fracture. Some patients may already be aware that they have a vertebral
fracture because of previous high impact trauma or they may be able to
provide information of severe high impact trauma in the past which may
have caused a vertebral fracture that was not identified at the time
(e.g. major motor vehicle accident causing back pain and patient was
bedridden for two weeks but no x-rays were done or available from that
incident). If, however, the historical details are ambiguous, referral
to an osteoporosis specialist may then be warranted.
Recommended
biochemical tests for patients being assessed for osteoporosis as per
the 2010 OC Guidelines: serum calcium corrected for albumin or ionized
calcium, complete blood count (CBC), creatinine or eGFR, alkaline
phosphatase, thyroid stimulating hormone (TSH). For patients with
vertebral fractures, a serum protein electrophoresis is also
recommended. Vitamin D (25-hydroxy vitamin D) should be measured after
3-4 months of adequate supplementation and should not be repeated if
optimal level ≥ 75 nmol/L is achieved.
Once
a vertebral fracture has occurred, it will always continue to appear as
such on all future x-rays. As a result, many vertebral fractures are
identified long after they initially took place and are of undetermined
age. For example, a painless vertebral fracture identified on x-ray for
the first time today, may have occurred 20 years ago, or yesterday.
When no prior x-rays are available and there is no clinical history to
suggest when the patient sustained the vertebral fracture, there is no
simple method to determine the exact time the fracture occurred. In
this algorithm, such fractures of undetermined age are assumed to be
old and to have occurred prior to the initiation of osteoporosis
treatment, unless there is evidence to the contrary.
Vertebral
(spine) fractures are the most common type of osteoporotic fracture and
yet, they are the most difficult to identify. Two thirds of them do not
cause the type of pain that would normally lead a patient to seek
medical attention. Consequently, vertebral fractures are usually found
as an incidental finding on x-rays done for other reasons (e.g. chest
x-ray to rule out a pneumonia). The assessment and management of spine
fractures can prove to be quite challenging. For this reason, many FLS
will integrate the spine fractures only after the protocols for hip and
non-hip non-spine fractures are well established.
Adequate
vitamin D supplementation is important, not only for bone health, but
also because it has been proven to reduce the risk of falls and
fractures. Osteoporosis Canada recommends vitamin D supplementation
of 800-2000 IU/day for adults ≥ 50 years of age.