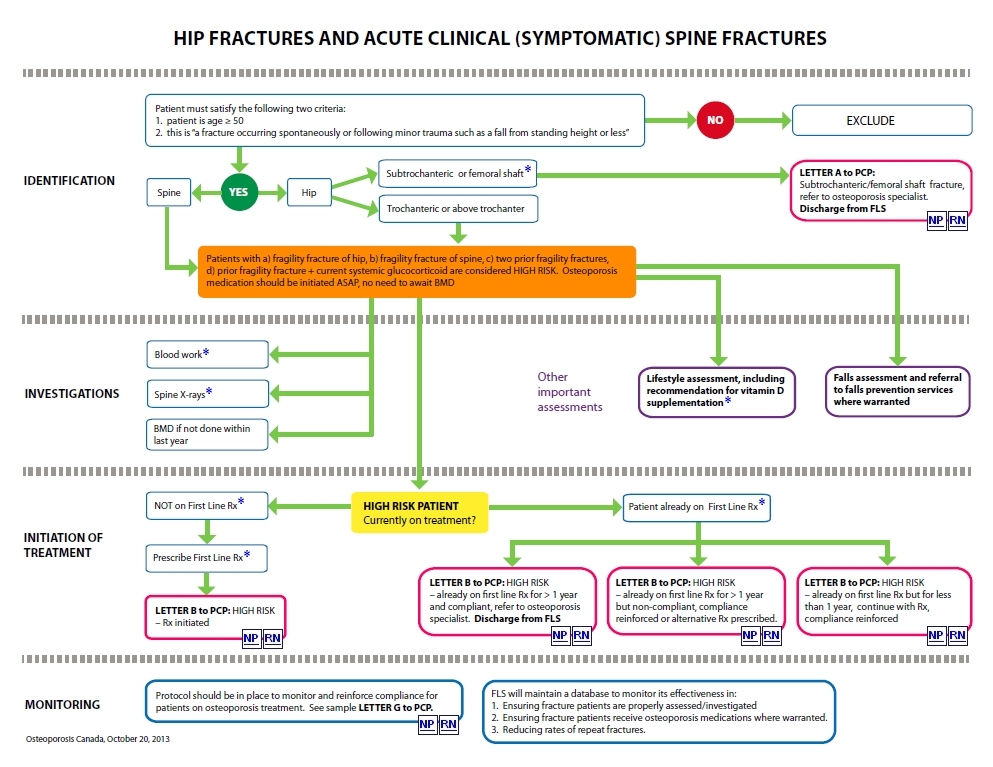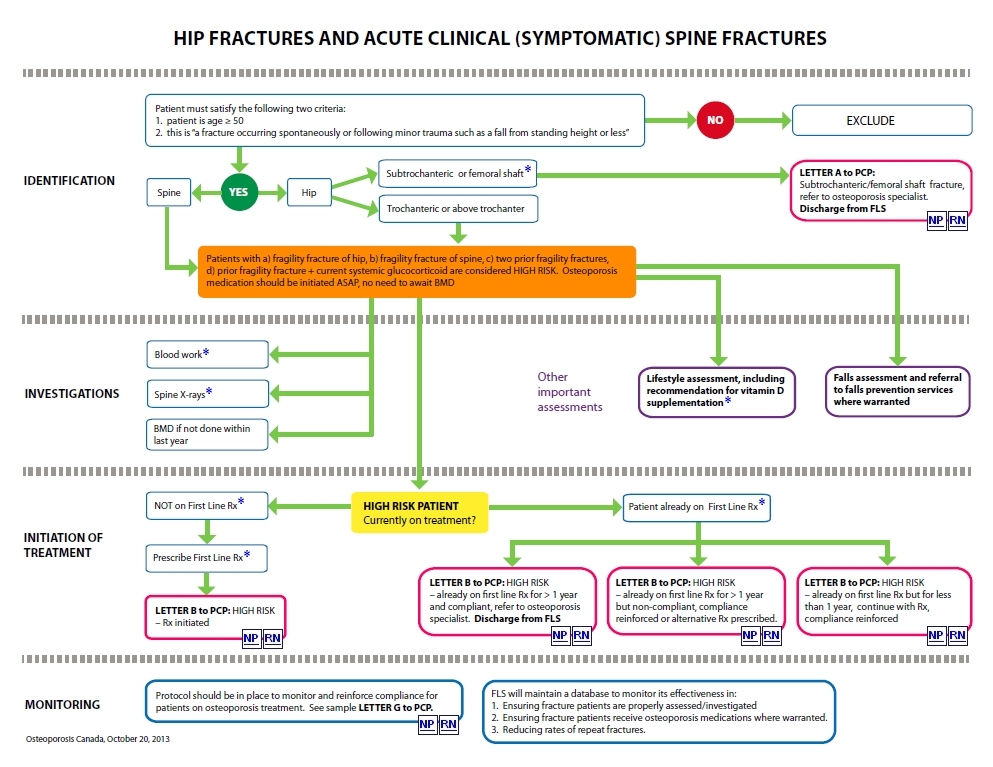
Subtrochanteric/femoral
shaft fragility fractures can be due either to osteoporosis or to prior
exposure to bisphosphonates. The assessment of such fractures is
complicated and warrants referral to an osteoporosis specialist.
Recommended
biochemical tests for patients being assessed for osteoporosis as per
the 2010 OC Guidelines: serum calcium corrected for albumin or ionized
calcium, complete blood count (CBC), creatinine or eGFR, alkaline
phosphatase, thyroid stimulating hormone (TSH). For patients with
vertebral fractures, a serum protein electrophoresis is also
recommended. Vitamin D (25-hydroxy vitamin D) should be measured after
3-4 months of adequate supplementation and should not be repeated if
optimal level ≥ 75 nmol/L is achieved.
The
IOF Best Practice Framework indicates that patients with any fragility
fracture should be assessed for the presence of spine fractures. This
requires a lateral view of the thoracic and lumbar spine, typically by
conventional x-rays or, where available, by Vertebral Fracture
Assessment (VFA) by DXA. If the initial presenting fracture is a
vertebral fracture, it is important to ensure that the entire spine is
imaged (e.g. if a T10 fracture is identified on a lateral chest x-ray,
then a lateral view of the lumbar spine is also indicated).
Adequate
vitamin D supplementation is
important, not only for bone health, but also because it has been
proven to reduce the risk of falls and fractures. Osteoporosis Canada
recommends vitamin D supplementation
of 800-2000 IU/day for
adults ≥ 50 years of age.